On August 2, 2018, the Centers for Medicare & Medicaid Services (CMS) issued a final rule that was intended to empower patients through better access to hospital price information. Current laws already required hospitals to make public a list of their standard charges, but the new requirement which became effective on January 1, 2019, required hospitals to publish a list of all charges in machine readable format via the internet, in an XML or CSV format. The final rule also required providers to update their posted charges no less than one time per year.
In recent months, CMS has further clarified the minimum requirements that hospitals not only publish their charge description master (“CDM”) but also publish their average charges by DRG and their drug prices, even if not provided for in their CDM.
Now that we are approaching the close of the second quarter of 2019, is this pricing transparency requirement much ado about nothing or a precursor of much more to come. The early signs from CMS indicate the latter.
Since the beginning of 2019, it has not been uncommon to see daily articles related to Pricing Transparency. At the forefront of this attention, has been U.S. Centers for Medicare and Medicaid Services Administrator, Seema Verma. She has been quoted as saying that “it is incumbent on every American to take control of their health care, to seek out high-value care from providers who are competing for their business, to demand their health-care information, and to make decisions that will lead to better, healthier lives.” In January, Ms. Verma took to Twitter and created the hashtag #WheresThePrice, where she challenged Twitter users to visit their local hospital website to find out if the hospital had posted their prices in an electronic format and to tweet her back. Since the CMS transparency requirement did not have an enforcement aspect, we saw how social media helped CMS drive accountability.

Recently, the Trump administration has suggested that providing payer-provider negotiated rates to the public might be beneficial to consumers in the future. Publishing these rates can easily throw the future years provider reimbursement scenario into a tailspin as payers and providers for the first time may see drastic and perhaps inexplainable differences in rates for like services and from the same or similar payers. Such a scenario might place pressure on payers to level out the rates they negotiate with providers placing some at risk financially.
Furthermore, as consumers are encouraged by CMS to shop hospital charges or rates what will the future be for inner city or inner-city teaching hospitals which in most cases will have much higher charges and rates? Clearly the healthcare community must stay on top of this issue by providing comments to CMS, ensuring that their pricing methodology and practices are based on sound, defensible methodologies but also begin to look at the consistency of their negotiated rates for like procedures and how to understand how those rates compare to the related procedure costs inclusive of overhead, bad debt and a reasonable margin.
Many valid arguments have been made around the imperfect nature of the pricing transparency requirements:
- Standard prices in the chargemaster may be confusing to patients due to the different levels of patient acuity and/or bundling of services
- Many providers already comply with the ACA requirements and consumers are simply not utilizing the processes in place to ascertain their cost information
- This information should be coming from health plans and hospitals should be focusing on the uninsured and out-of-network patient costs
Despite the validity of these arguments, compliance with pricing transparency is not optional and should be taken seriously by the leadership of your healthcare organizations.
What should healthcare providers do to comply with the pricing transparency requirements?
Below is a simple decision tree that helps you determine some of the minimum requirements along with other steps that go above and beyond the CMS requirements but may make the data more useful and accessible to your patients/customers.
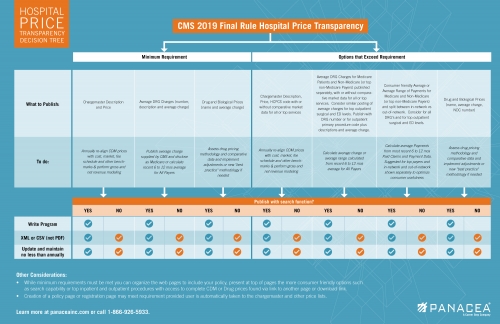
As seen from this decision tree, the minimum requirements include publishing your chargemaster prices, average DRG charges and drug and biological prices. Prior to publishing any of this information, at a minimum, the following is recommended:
- Re-align CDM prices annually with consideration to cost, market, commercial, managed care and governmental fee schedules and other benchmarks or a hybrid thereof. In addition, gross and net revenue modeling of the new prices is highly beneficial in order to reduce the risk of unintended impacts to your bottom line.
- Determine if your organization should simply publish the average charge by DRG provided by CMS or calculate a 6 to 12-month average for all payers or segregated between Medicare and Non-Medicare payers.
- Assess your drug pricing methodology and comparative data, perform modeling and accordingly implement adjustments or new “leading practice” methodology if needed.
Options that go above and beyond the minimum requirements would be to supplement the data with average charge profiles for inpatient and outpatient procedures. This might include average DRG charges and average per case charges for top outpatient procedures illustrated separately for Medicare Patients and Non-Medicare (or top non-Medicare Payers) and with or without comparative market data. For example, a consumer can see what a hip or knee replacement may cost and what average low, medium, high charges might be for a specific payer. Further segregating between average charges per case between in-network and out-of-network status would also provide improved disclosure in this era where out-of-network patients are often blind-sided by their balances due. We would suggest using at least 6 to 12 months of recent claims data to calculate these amounts. Going further beyond the CMS requirement your organization can consider providing a more consumer friendly web experience that includes a search functionality by description or code. A decision would then have to be made to write a program in-house or have a vendor assist to develop one. If the search function is not feasible for your organization, then you can just publish or list your charges.
Pricing Transparency is here to stay
Pricing Transparency is here to stay, and those providers that are proactive in developing defensible pricing practices coupled with a patient-friendly communication strategy will be able to navigate these new requirements efficiently and effectively. This is only the beginning as CMS is considering the requirement to also publish your payer rates and has begun research on the feasibility of implementing a dynamic bidding system to help consumers choose where they have their healthcare service provided. Providers are encouraged to use this time wisely to understand their procedure level costs and profitability, the reasonableness of their rates and charges as compared to fully allocated costs inclusive of a reasonable margin and their competitive position.
Download a copy of the decision tree.
[1] A PDF file format is not considered machine readable



